
On the evening of April 10th, the Centers for Medicare and Medicaid Services released three proposed rules. These rules include proposals related to payment, quality reporting, and other areas for skilled nursing facilities (SNFs), inpatient psychiatric facilities, and hospices.
Comments on the proposed rules are due on June 9, 2020.
Total Payments to SNFs to Increase in FY 2021
The prospective payment system (PPS) for skilled nursing facilities (SNFs) uses a case-mix classification system called the Patient Driven Payment Model (PDPM) for classifying SNF patients. The PDPM classifies patients into groups based on patient-characteristics instead of using volume of therapy services as the basis for payment classification and has been implemented in a budget neutral manner.
CMS is proposing the following unadjusted federal rate per diems:
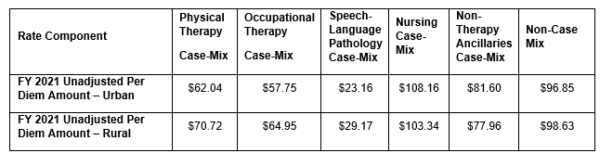
Overall, CMS is estimating that payments to SNFs in FY 2021 will increase by $784 million from the annual PPS payment rate update. For FY 2021, CMS is proposing a SNF market basket update factor of 2.3 percent, which accounts for the market basket increase factor of 2.7 percent less the 0.4 percentage point multifactor productivity adjustment. SNFs that fail to report the required quality data will have a 2 percent reduction applied to their payments.
No updates are being proposed on the performance period or payment policies for the SNF Value-Base Purchasing Program (SNF VBP). CMS is also not proposing any changes to the Skilled Nursing Facility Quality Reporting Program (SNF QRP).
CMS Proposes to Adopt Revised Delineations for Geographic Designations
The Office of Management and Budget (OMB) established revised delineations for Metropolitan Statistical Areas (MSAs), Micropolitan Statistical Areas, and Combined Statistical Areas in a September 2018 bulletin. CMS is proposing to adopt these updates to the OMB delineations for the SNF PPS effective beginning FY 2021. The agency believes that 34 counties currently considered urban would now be considered rural and 47 rural counties will become urban.
To prevent any major disruptions, CMS is proposing a 5-percent cap on any decreases in a SNF’s wage index for FY 2021 to allow the effects of the revised delineations to be phased in. A budget neutrality factor will be applied to federal per diem rates to account for the estimated effect of the changes to the wage index values.
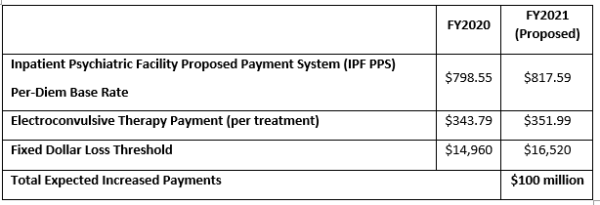
Inpatient Psychiatric Payment Rates Set to Increase +2.6% for 2021
CMS is proposing to increase both the per-diem base rate as well as per-treatment payments for electroconvulsive therapy in 2021, which the agency predicts will result in $100 million in additional spending. Inpatient psychiatric facilities are paid a daily base rate intended to cover all routine, ancillary, and capital costs. The per-diem payment may be adjusted based on a patient’s Diagnosis-Related Group (DRG) assignment and comorbidities. Payments are also adjusted to reflect higher expenses at the beginning of a patient’s stay and lower expenses towards the later days of the stay.
CMS is not proposing any changes to the Inpatient Psychiatric Facilities Quality Reporting (IPFQR) Program for 2021.
Hospice Payment Rates Set to Increase +2.6% for FY 2021
The proposed payment rule for hospices includes a proposed payment increase of 2.6 percent for FY 2021, proposes to sunset the service intensity add-on budget neutrality factor, and proposes a 5 percent cap on wage index decreases. Hospices that fail to report the required quality data will have a 2 percent reduction applied to their payments. CMS estimates $580 million in increased payments to hospices in FY 2021.
The proposed rule includes a transition policy of a 5% cap on any decrease in a geographic area’s wage index value from the prior FY to help mitigate any significant negative impacts that hospices may experience in the proposed adoption of the Office of Management and Budget (OMB) delineations to update the hospice wage index.
CMS is soliciting comments on model examples of the modified hospice election statement and the addendum that were finalized in the FY 2020 Hospice final rule. Beginning October 2021, hospices, upon request, must furnish an election statement addendum that lists non-covered items, services, and drugs.
CMS is not proposing any changes to the Hospice Quality Reporting Program for 2021.
