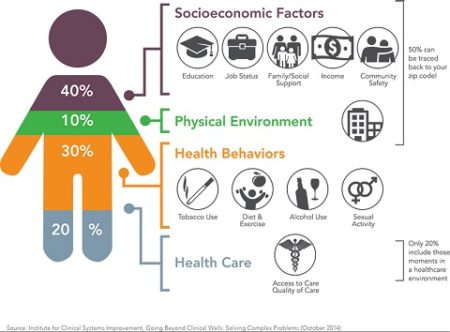
Recent announcements from two giants in the healthcare field offer important insights into the growing focus on the social determinants of health, or SDOH, as they are widely known. According to the CDC, these social determinants are “economic and social conditions that influence the health of people and communities” and are shaped by the amount of “money, power and resources that people have.” The CDC itemizes these factors as early childhood education, employment, the type of work of a person does, access to food, access to health services and the quality of those services, housing, income, discrimination and social support. The absence of these factors in an individual’s life can negatively impact their health. So current approaches are looking beyond the immediate short-term issues in a patient’s care, to the total environment impacting their well being.
For instance, last April, United Healthcare announced that it has invested more than $400 million to increase affordable housing access for people in underserved communities. At the time of the announcement, the company stated that “when homeless people have access to stable housing, they can manage their health more effectively.” More recently, Kaiser Permanente launched “Food for Life”; a program that it says will provide vulnerable patients access to nutritious meals. Like the United Healthcare program, the Kaiser approach is ultimately designed to provide better patient care and lower healthcare costs
The realization that social factors can negatively impact health outcomes has been growing over the past decade. Kaiser and Unitedhealthcare are hardly alone in launching programs to try to neutralize or reverse their impact. According to the Harvard Business Review, these programs have grown ten-fold over the past decade, with varying rates of success. But as hospital administrators, state Medicaid programs, and large insurers constantly search for innovative ways to cut healthcare costs, the SDOH programs are expected to become integral parts of the healthcare system.
Our health care system is appropriately sharpening its focus on the social factors that can diminish an individual’s chances to enjoy good health. The tough questions moving forward will focus on finding out which programs are effective, and financially sustainable. To help generate data that will point to successful programs, the Centers for Medicare & Medicaid Services (CMS) is sponsoring the Accountable Health Communities Model to “test whether systematically identifying and addressing the health-related social needs of Medicare and Medicaid beneficiaries will impact health care costs and reduce health care utilization.” This public sector effort, as well as the private sector efforts to alleviate social conditions that drive up health costs, could begin to clarify the best systemic approaches. Anyone involved in the delivery of health care to the American population would do well to closely watch their results.
